Written by: Banyan Editorial Staff | Medically reviewed by: Dr. Darrin Mangiacarne - Chief Medical Officer | Edited: February 2025
Addressing Co-Occurring Disorders at Banyan
Addiction is a terrible disease. It can lead to severe health problems, unsightly physical effects, relationship problems, and even legal issues, but for some people, the problems do not stop there. If you find that you or a loved one is struggling with poor mental health on top of a drug or alcohol issue, Banyan’s dual diagnosis treatment centers can help.
Dealing with a substance use disorder is challenging enough on its own, but unfortunately, addiction is often accompanied by other troubles as well. An estimated 7.7 million adults in the United States suffer from both a substance use disorder as well as a mental illness, known as a co-occurring disorder.
What Is Dual Diagnosis?
Dual diagnosis, also known as a co-occurring disorder, is the term used to describe an individual who is suffering from a substance abuse disorder as well as a mental health disorder simultaneously. Dual-diagnosis disorders are often difficult to diagnose or may be misdiagnosed due to the complexity of the symptoms. It can also sometimes be difficult to determine which problem came first. Many people struggling with mental health problems will turn to drugs or alcohol to self-medicate and will develop a substance abuse problem as a result.
Others may develop a mental health disorder after they already have an addiction. According to the 2018 National Survey on Drug Use and Health, over 9 million Americans struggled with both a mental illness and a substance abuse problem that past year. If you or someone you know has been experiencing these issues, a dual-diagnosis treatment program could make all the difference.
Warning Signs of a Dual Diagnosis
When two diseases are present at the same time, it can be hard to manage the active symptoms. There can be an overlap when it comes to the symptoms of depression and the symptoms of alcoholism and it’s important to seek professional treatment for a proper diagnosis. The signs and symptoms of dual diagnosis will vary depending on the diseases present. If you are worried that your loved one is suffering from a co-occurring disorder, look for these warning signs.
- Daily functioning is almost impossible
- Inability to keep a job
- Healthy relationships are being destroyed
- Extreme mood changes and frequent outbursts at people
- Irritability and restlessness
- Financial struggles
- Engaging in risky behavior
- Employment Problems
In addition to these signs, consider these more specific symptoms that might indicate a dual diagnosis:
- Sudden behavior changes: Rapid shifts in behavior can signal underlying issues.
- Difficulty managing daily tasks: Basic responsibilities can become overwhelming.
- Retreating from relationships: Withdrawal from family and friends is common.
- Neglecting health and hygiene: A noticeable decline in self-care routines.
- Developing high tolerance to a substance: Needing more of the substance to achieve the same effect.
- Feeling the need to use the substance to function normally: Reliance on substances for day-to-day activities.
- Experiencing withdrawal symptoms: Physical or mental symptoms when the substance is not used.
These comprehensive warning signs are crucial for recognizing when dual diagnosis might be an issue. Remember, only a mental health professional can provide a proper diagnosis, but understanding these symptoms can be a vital first step in seeking help.
What Steps Can I Take if I Suspect I Need Dual Diagnosis Treatment?
If you find yourself struggling with both mental health issues and substance use concerns, it may be time to consider dual diagnosis treatment. Here’s how you can take actionable steps towards getting the right support:
-
Consult Your Primary Care Physician
Begin by discussing your concerns with your regular doctor. They can provide a comprehensive evaluation, offer insights into your symptoms, and suggest immediate steps or referrals. -
Seek Professional Mental Health Advice
Reach out to a licensed mental health professional such as a psychologist or psychiatrist. They specialize in diagnosing and treating co-occurring disorders and can tailor a treatment plan to your unique situation. -
Research Treatment Facilities
Look into treatment centers that specialize in dual diagnosis programs. Consider facilities that are well-reviewed and have a track record of treating both mental health and substance use disorders effectively. -
Engage with Peer Support Groups
Join groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA). While these aren't specifically for dual diagnosis, they can provide support and help connect you with others who understand your challenges. -
Utilize Helpline Resources
Contact national hotlines such as the Substance Abuse and Mental Health Services Administration (SAMHSA). They can guide you through available options and help you find the right treatment resources in your area.
Taking these steps can lead you towards finding the support and care you need, helping you navigate the complexities of dual diagnosis treatment.
Is Dual Diagnosis Treatment Right for Me?
Determining whether dual diagnosis treatment is suitable for you depends on your individual health circumstances. This specialized form of treatment is ideal for those who are managing both a mental health disorder and a substance use disorder simultaneously. Addressing these conditions together can offer a more comprehensive path to recovery.
Why Consider Dual Diagnosis Treatment?
-
Holistic Approach: Treating both mental health and substance use issues concurrently ensures that neither condition is neglected. This can lead to a more thorough and effective recovery process.
-
Integrated Care: By addressing the intricate connection between mental health and addiction, dual diagnosis treatment provides integrated care that acknowledges how these conditions affect each other.
Steps to Determine Suitability:
-
Consult Healthcare Professionals: Speak with your primary care doctor or a licensed mental health professional. They can offer insights based on your medical history and current condition.
-
Mental Health Evaluation: A comprehensive assessment by a mental health specialist can confirm if dual diagnosis treatment is necessary for you.
-
Rehabilitation Programs: Explore various rehabilitation programs that specialize in dual diagnosis. Reach out to licensed facilities and inquire about their approach and success stories.
Ultimately, if you suspect that your mental health struggles are intertwined with substance use, seeking dual diagnosis treatment could be a pivotal step towards health and well-being.
Questions about our Facilities or Programs?
Our admissions coordinators are available 24/7 to answer any questions you may have as you consider whether treatment at Banyan is right for you or your loved one.
The Co-occurring Disorders We Treat
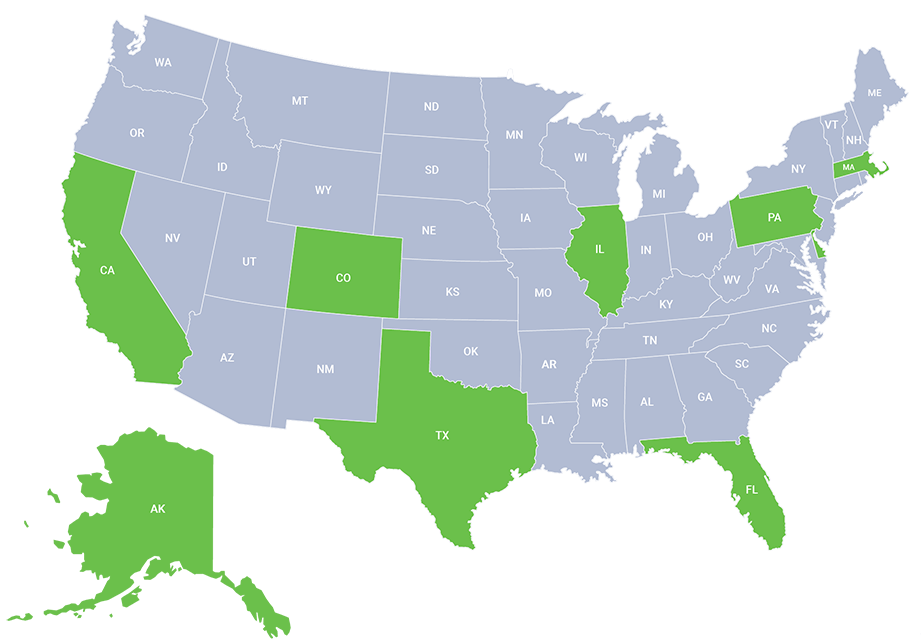
At our nationwide treatment centers, we understand that addiction often isn’t just about the body’s dependence on a drug.
Because every person’s problems are unique, treatment for a co-occurring disorder needs to be tailored to the patient for a comprehensive approach. We work to create a personalized treatment plan so that patients can not only overcome their addictions but also improve their mental health in the process. During their time with us, patients will participate in numerous different treatment programs and therapies designed to meet their specific needs.
Comprehensive treatment is essential for facilitating the best outcomes for individuals with co-occurring disorders. Here's how our approach benefits patients:
-
Substance Use and Mental Health: Patients receive the necessary treatment to stop using drugs or alcohol while simultaneously engaging in therapy to manage their mental health disorders. This dual focus ensures that both aspects of their diagnosis are addressed.
-
Understanding Connections: Through personalized therapy sessions, patients work with therapists to understand how their disorders are interconnected. This insight is crucial for addressing the root causes of both addiction and mental health issues.
-
Coping and Prevention: Patients learn coping mechanisms tailored to their mental health conditions and develop skills to identify and avoid triggers associated with relapse. Building a solid relapse prevention plan is a key component of our program.
-
Motivation and Engagement: By increasing their motivation for engaging in treatment, we empower patients to take active roles in their recovery journey, enhancing their chances of long-term success.
Our comprehensive approach not only tackles each disorder individually but focuses on the broader picture, ensuring patients leave with the tools and understanding necessary to maintain their recovery and improve their overall well-being.
Our dual-diagnosis treatment centers can handle a variety of co-occurring disorders, including:
- Depression and Substance Use Disorder
- When depression symptoms last over at least two weeks and start to interfere with normal life, this is when the depressive state can be an issue.
- Anxiety/Panic Attacks and Substance Use Disorder
- Anxiety and/or Panic disorder and addiction treatment plans come with intense therapy sessions including individual and group settings, education on both the anxiety or panic disorder and disease of addiction, family support groups, relapse prevention, and more.
- Bipolar Disorder and Substance Use Disorder
- Bipolar disorder is known as one of the more serious mental health disorders that is characterized by intense and sudden mood changes, drastic energy level changes, and erratic and irrational behavior.
- Attention Deficit Hyperactivity Disorder and Substance Use Disorder
- Attention Deficit Hyperactivity Disorder (ADHD), formerly known as Attention Deficit Disorder (ADD), is a behavioral disorder often diagnosed at a young age. There is an assumption that those with ADHD are more prone to addiction due to early prescription of stimulant medications like Adderall and Vyvanse, which can be addictive. In some dual-diagnosis cases, the mental disorder leads to self-medication with alcohol or drugs, potentially causing addiction. Full-blown addiction can have devastating results, making it crucial to treat both the addiction and behavioral disorder concurrently for sustained recovery. At our treatment center, we provide individualized programs to address the symptoms of both disorders.
- Obsessive-compulsive disorder (OCD) is an anxiety disorder characterized when an individual experiences repetitive and recurring thoughts that cause anxiety and irrational fears.
- With individual and group therapy sessions, patients will explore the relationship between their addiction and mental health problems with a licensed therapist and peers struggling with similar issues. We work to create a personalized treatment plan so that patients can not only overcome their addictions but also improve their mental health in the process. During their time with us, patients will participate in numerous evidence-based and holistic treatment programs and therapies designed to meet their specific needs.
What Are the Risks of a Dual Diagnosis?
A person's health can be seriously affected by the complex combination of risks that come with having two diagnoses. The first problem with a dual diagnosis is that it might lead to approaches to therapy that are ineffective since symptoms of one ailment can mirror or be misunderstood for those of another. Moreover, the complex interaction that can arise between substance abuse and mental health problems makes people with two disorders much more prone to relapse. Treatment attempts may be complicated if both disorders are present, making it more difficult to find appropriate treatments. There is also a greater likelihood of self-medication, which involves using medications to address mental illness symptoms. This poses a risk to one's overall health. Social isolation, stigma, and difficulties in accessing suitable care also contribute to the elevated risks associated with dual diagnosis. Overall, addressing these complex interrelationships is crucial for effective treatment and recovery.
What Is the Dual Diagnosis Model of Treatment?
During dual diagnosis treatment, the patient will receive an initial medical assessment that will determine the best rehab program and type of treatment needed. At our nationwide treatment facilities, we provide customized treatment programs, and our clinicians and therapists are committed to fully treating and healing each patient for long-term success. Through unique addiction therapy methods and evidence-based treatment, a patient will be able to overcome both diseases and learn the tools needed to handle everyday situations in recovery. Additionally, patients are taught to actively practice relapse prevention techniques outside of treatment, minimizing the chances of a relapse. Implementing a dual diagnosis model in addiction treatment centers is crucial for providing comprehensive and effective care.
Dual diagnosis treatment offers a comprehensive approach to addressing both mental health and substance use disorders, ensuring that neither is neglected. The benefits include:
- Customized Care: Patients receive tailored treatment programs designed to address their specific needs, enabling a more personalized recovery journey.
- Integrated Therapy: Therapy sessions help individuals understand the interplay between their mental health and substance use, providing insights into how these conditions are connected.
- Root Cause Analysis: Treatment delves into the underlying causes of addiction and mental health disorders, fostering a deeper understanding and promoting holistic healing.
- Coping Strategies: Individuals learn effective coping mechanisms to manage their mental health conditions, enhancing their ability to handle stress and triggers.
- Trigger Identification: Patients are guided to identify and avoid triggers associated with relapse, developing robust strategies to maintain sobriety.
- Relapse Prevention Planning: A strong focus is placed on building a solid relapse prevention plan, equipping patients with the tools necessary for sustained recovery.
- Motivation Enhancement: Treatment aims to increase patients' motivation for engaging in and committing to their recovery process.
This dual-focused approach not only addresses immediate issues but also empowers individuals for long-term success in their recovery journey. By comprehensively tackling both disorders, patients are better prepared to reclaim their lives and maintain lasting wellness.
Here's an overview of the key aspects:
- Integrated Approach:
- Recognizes the interplay between substance use and mental health disorders.
- Provides a seamless integration of treatment for both conditions within the same therapeutic framework.
- Simultaneous Treatment:
- Addresses both substance use and mental health issues concurrently rather than treating them in isolation.
- Aims to achieve a holistic understanding of the individual's unique challenges and needs.
- Comprehensive Assessment:
- Conducts a thorough assessment to identify and evaluate both substance use and mental health disorders.
- Considers the impact of one condition on the other to inform a tailored treatment plan.
- Customized Treatment Plans:
- Develops individualized treatment plans that address the specific needs and challenges of each person.
- Combines evidence-based interventions for substance use and mental health disorders.
- Collaborative Care:
- Involves a multidisciplinary team of professionals, including addiction specialists and mental health professionals.
- Promotes collaboration between treatment providers to ensure cohesive and coordinated care.
- Psychoeducation:
- Provides education about the relationship between substance use and mental health disorders.
- Helps individuals understand how one condition may influence or exacerbate the other.
- Dual-Focused Therapies:
- Utilizes therapeutic modalities that are effective for both substance use and mental health issues.
- Includes cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and other evidence-based approaches.
- Relapse Prevention:
- Integrates relapse prevention strategies that address both substance use triggers and mental health challenges.
- Empowers individuals with coping skills to navigate stressors without resorting to substance use.
- Ongoing Monitoring:
- Continuously monitors progress in both substance use and mental health treatment.
- Adjusts the treatment plan as needed to address evolving needs.
The Dual Diagnosis Model of Treatment aims to break the cycle of recurrent issues by providing comprehensive, integrated, and individualized care.
Getting into treatment is easy with our free insurance verification
"*" indicates required fields
The Importance of a Relapse Prevention Plan
In the realm of dual diagnosis treatment, relapse prevention is a crucial aspect of recovery. An individual's relapse prevention plan acts as a road map for navigating the obstacles and triggers that may appear along the way to recovery. It offers a structured framework that enables people to recognize potential threats, create coping mechanisms, and maintain their advancement through time.
The ability of a relapse prevention plan to address the intricate interactions between mental health and substance addiction is one of the primary reasons why it is essential for people with co-occurring illnesses. The symptoms of one illness frequently worsen the symptoms of the other in co-occurring disorders. Individuals can establish individualized strategies to manage both elements of their substance use and mental health by developing a thorough relapse prevention plan. By doing so, they can obtain a greater awareness of the complex relationships that exist between their mental health symptoms and substance use.
Relapse prevention strategies also give people a sense of empowerment and self-efficacy. It enables individuals to reclaim control over their lives and gives them the skills they need to overcome obstacles. People can increase their resilience and improve their capacity to fend off relapse by recognizing possible triggers, putting healthy coping strategies into practice, and putting in place a support network. Relapse prevention plans are proactive measures that enable people to take control of their recovery and make decisions that are in line with their long-term objectives and general well-being.
Get Started with Dual-Diagnosis Treatment
If you or someone you know is struggling with a mental health disorder and substance abuse, help is just a phone call away. Our nationwide drug and alcohol rehab could lead you or a loved one to a life free from drugs or alcohol and with improved mental health. Contact us today at (888) 981-7763.
Explore Your Options for Finding a Facility
Finding the right dual diagnosis treatment facility is crucial for comprehensive care. Here are several ways to locate the best option for your needs:
-
Reach Out for Immediate Assistance: Call the Substance Abuse and Mental Health Services Administration’s helpline at 1-800-662-HELP (4357) for guidance and support.
-
Utilize Online Tools: Use a behavioral health treatment locator tool to search for facilities equipped to handle dual diagnosis cases.
-
Consult Healthcare Professionals: Ask your doctor or therapist for personalized recommendations on rehab centers that specialize in dual diagnosis treatment.
-
Localize Your Search: Search for recovery resources by entering your zip code to find nearby centers offering the care you need.
Taking the first step towards recovery can be daunting, but with these resources, you can find the support necessary to embark on a journey towards better mental health and sobriety.
Frequently Asked Questions
Inpatient Dual Diagnosis Treatment:
- Requires individuals to stay at a dual diagnosis rehab facility for a structured, intensive program.
- Provides 24/7 medical supervision, therapy, and mental health care.
- Ideal for individuals with severe co-occurring disorders or those needing a stable environment for recovery.
Outpatient Dual Diagnosis Treatment:
- Allows individuals to live at home while attending therapy and treatment sessions.
- Suitable for those with a strong support system and mild to moderate co-occurring disorders.
- Provides flexibility for work, school, or family responsibilities.
Choosing between inpatient and outpatient treatment depends on the severity of the disorder, personal circumstances, and medical recommendations from dual diagnosis treatment centers near me.
- Banyan Boca
1000 NW 15th St
Boca Raton, FL 33486 - Banyan Castle Rock*
1055 S Perry St,
Castle Rock, CO 80104 - Banyan Gulf Breeze*
4400 Hickory Shores Blvd,
Gulf Breeze, FL 32563 - Banyan Philadelphia*
100 N Bucks Town Dr Suite 100E,
Langhorne, PA 19047 - Banyan Pompano*
950 N Federal Highway
Pompano Beach, FL 33062 - Banyan Sebring
1062 Lake Sebring Dr,
Sebring, FL 33870 - Clearbrook Massachusetts*
83 Hospital Road,
Baldwinville, MA 01436 - Behavioral Health of the Palm Beaches*
7859 Lake Worth Rd,
Lake Worth, FL 33467

Related Reading:
Sources: