In the realm of substance abuse and addiction, understanding the physical and psychological impact of opioids is essential for effective treatment and recovery. Opioids, a class of potent pain-relieving medications, have the potential to linger in the human body, influencing various physiological processes. In this article, the experts of our addiction treatment facilities delve into the intricate details of the duration opioid drugs remain in your system, shedding light on the factors that contribute to their persistence. With a commitment to fostering awareness and promoting informed decision-making, Banyan Treatment Centers offers valuable insights into the critical question: How long do opioids stay in your system? This exploration aims to empower individuals, their families, and healthcare professionals with knowledge that is pivotal in the pursuit of a healthier, substance-free life.
Break Down of How Opioids Work
Opioids work by interacting with mu-opioid receptors in the brain and body. The body's natural pain management system includes these receptors, which opioid medications activate to generate a range of effects, such as relief from pain and a feeling of well-being. Since endorphins are naturally occurring chemicals in the body that bind to these receptors, opioids operate mainly by imitating their actions.
Here is a breakdown of how opioids function:
- Receptor activation: The brain, spinal cord, gastrointestinal tract, immune system, and other tissues all contain mu-opioid receptors, which are the specific receptors that opioids bind to.
- Pain relief: By binding to these receptors, opioids reduce the perception of pain. They inhibit the transmission of pain signals along the spinal cord and alter the brain's interpretation of pain.
- Euphoria and relaxation: Opioids can also produce a sense of euphoria and relaxation. This is due to their impact on the reward centers of the brain, where they increase the release of dopamine, a neurotransmitter associated with pleasure.
- Respiratory depression: One significant side effect of opioids is respiratory depression, where the rate and depth of breathing decrease. This effect can be dangerous, especially at higher doses.
How Long Does It Take for Opioids to Kick In?
The onset of action for opioids, or the time it takes for them to "kick in," can vary depending on the specific opioid and its formulation. Generally, opioids work relatively quickly to alleviate pain and produce their desired effects. The onset of immediate-release opioids is typically within 15 to 30 minutes after ingestion. On the other hand, extended-release formulations, designed for a more gradual release of the medication over an extended period, may take several hours to reach their peak effectiveness.
It's important to keep in mind that a person's metabolism, general health, and the presence of other substances in the body can all have an impact on how quickly opioids take effect. As such, you should always follow prescribed dosages and guidelines to minimize the risk of adverse effects. If you have specific concerns or questions about a particular opioid medication, consult with a healthcare professional.
Factors That Affect How Long Opioids Stay in Your System
The duration of opioid use in the body may differ based on a variety of factors. The duration of opioid presence is influenced by individual variations, the specific opioids taken, and various biological and lifestyle factors.
Here are key factors that may impact how long opioids remain in your body:
- Type of opioid: The half-life of different opioids varies, affecting the speed at which the body breaks down and releases them. Short-acting opioids may clear the system more rapidly than long-lasting ones.
- Dosage and frequency of use: Taking opioids more often and at higher doses could lead the body to build up them, which takes longer to be eliminated.
- Metabolism: The rate at which an individual breaks down and eliminates opioids differs based on their metabolic makeup. Quicker clearance might be the result of a faster metabolism.
- Liver function: The breakdown of opioids is primarily reliant on the liver. Opioid clearance from the body may be inhibited if liver function is impaired.
- Kidney function: The kidneys are frequently utilized in the elimination of opioids and their metabolites. Opioid elimination can be affected by impaired kidney function, especially when it comes to medications that are mostly eliminated by urine.
- Hydration levels: The body's normal detoxifying actions are helped by sufficient hydration. Dehydration can lead to the elimination of opioids to occur more slowly.
- Age: As people age, their rate of metabolism tends to slow down. This may have an impact on how quickly opioids are eliminated from the body, particularly in older people.
- Body mass index (BMI): The amount of body fat can affect the way opioids circulate and are stored. Since opioids are lipophilic or soluble in fat, people who have greater fat percentages may be able to break down the medications more slowly.
- Genetics: Genetic variables can affect drug metabolism and variations in the rate at which opioids break down and are excreted.
- Overall health: Drug metabolism and elimination can be affected by an individual's overall health, including any underlying medical conditions.
It is essential to recognize that these factors interact in a complex way and that different people experience opioids in the body for various periods. For advice and information, talking with a medical professional is advised if there are worries about opioid use or its effects.
How Long Do Opiates Stay in Your System?
Opioids' half-life in your body can vary based on several factors, such as the particular opioid medication, dosage, frequency of use, metabolism, and individual variances. The following are some detection windows for biological samples within which opiates can be detected:
- Urine: After a single use, opioids are usually detectable in urine for 1 to 3 days. It may remain noticeable for a longer amount of time—up to several days or even a week—in chronic users.
- Blood: Compared to urine, opioids are typically detected in blood for a shorter period. After use, they might remain for up to 12 hours, though this might change.
- Saliva: Opioids are detectable in saliva for a shorter period, usually up to 2 days following usage.
- Hair: Opioids can remain in hair follicles for up to 90 days or longer. Hair testing is less common but frequently used to evaluate patterns of long-term drug use.
It is important to remember that these are only approximate values and that there may be individual differences. Several variables can affect how quickly opiates are metabolized and eliminated from the body, including liver function, hydration levels, and the presence of other substances. Furthermore, detection times may be impacted by more recent and accurate drug testing techniques.
For individualized and accurate information based on your unique circumstances, it is advised that you speak with a healthcare provider or a toxicology specialist if you have concerns about opiates and their presence in your system.
How Long Do Opioids Stay in Urine?
The specific opioid, the dosage, the frequency of use, and individual metabolic variances can all affect the detection window for opioids in the urine. The following are broad approximations for the opioid detection durations in urine:
- Short-acting opioids (e.g., heroin, hydrocodone, oxycodone):
- Single use: Detectable for approximately 1-3 days.
- Chronic use: Detectable for a longer period, up to several days or a week.
- Long-acting opioids (e.g., methadone, buprenorphine):
- Single use: Detectable for 1-7 days.
- Chronic use: May be detectable for an extended period, potentially up to a week or more.
It's crucial to remember that these are only rough estimates and that specific factors like metabolism, hydration levels, and general health can affect how long a detection takes.
How Long Do Opioids Stay in Your Blood?
When compared to other biological samples, such as urine, the duration of opioid detection in blood is typically shorter. The precise length of time may differ depending on the particular opioid, dosage, frequency of use, and individual metabolic variations. The following are broad approximations for the opioids' detection durations in blood:
- Short-acting opioids (e.g., heroin, hydrocodone, oxycodone):
- Detectable for approximately 6-12 hours after a single use.
- Long-acting opioids (e.g., methadone, buprenorphine):
- Detectable for a slightly longer duration, typically up to 24 hours after use.
Remember that these are only estimates and that actual detection times may differ depending on several variables, including liver function, metabolism, and the particular opioid in question. Furthermore, different people react differently to opioids, which can affect how long it takes for the drugs to leave the bloodstream.
Urine tests are more commonly used for routine opioid testing than blood tests because they can identify drug use over a longer period. When it's necessary to confirm recent drug use, like in cases of suspected impairment or overdose, blood tests are frequently used.
Toxicology experts or medical professionals should be consulted for precise and customized information regarding opioid detection in blood.
Do Opioids Stop Working After a While?
Yes, opioids may stop working the same way they initially did after a while of use. In other words, opioid users may become less responsive to the same dosage of the drug over time, making it less effective in eliciting the desired effects, such as euphoria or pain relief. As the body grows accustomed to the opioid, tolerance develops, and greater dosages might be needed to produce the same degree of effect.
Prolonged opioid use can also result in physical dependence, where the body adjusts to the opioid's presence and can cause withdrawal symptoms upon abrupt cessation, in addition to tolerance. While physical dependence is a common physiological reaction to regular opioid use, it is not the same as addiction.
Opioid tolerance does not always mean that opioids stop working entirely, even though tolerance and physical dependence are common. Nevertheless, the efficacy of opioids has its limits, and the risk of side effects and harms associated with opioid use can rise when dosages are continuously increased in an attempt to overcome tolerance.
It's critical to distinguish between the idea of opioid effectiveness and tolerance. For some people, opioids can still be used to effectively manage pain or achieve desired effects, but to reduce risks and address any signs of tolerance or dependence, healthcare professionals should closely monitor the management of opioid use.
It is important to speak with a healthcare provider if a patient is having problems related to tolerance or is worried about the efficacy of their opioid medication. Modifications to the treatment plan, such as taking into account alternate pain management techniques, may be considered to address these issues. Healthcare professionals can also guide people through possible hazards and assist them in making decisions about the use of opioids.
How Long Is Too Long on Opioids?
Determining how long is "too long" to take opioids is a complicated and personal choice that should be discussed with a healthcare provider. The nature and severity of the medical condition, the efficacy of pain management, the possibility of side effects, and the likelihood of developing tolerance and dependence are some of the factors that determine how long it is appropriate to use opioids.
Here are some things to consider when deciding how long opioids should be used:
- Acute vs. chronic pain: In most cases, opioids are useful and suitable for treating acute pain, such as pain following surgery or pain from trauma. However, the advantages and disadvantages of continuing opioid use for chronic conditions like persistent back pain must be carefully considered.
- Effectiveness of pain management: Opioids may be used for a longer amount of time if they can effectively manage pain and enhance quality of life without causing appreciable side effects. Ongoing evaluation of the treatment plan is essential, though.
- Risk of tolerance and dependency: Extended use of opioids can result in tolerance, which makes higher doses necessary to achieve the same result, and physical dependence, which causes withdrawal symptoms when stopped. Medical professionals keep an eye on these variables and may modify treatment regimens as necessary.
- Investigation of alternatives: The overall pain management plan should take into account and incorporate non-opioid and alternative techniques for chronic pain management. This could involve interventional procedures, non-opioid medications, and physical therapy.
- Addiction risk: Long-term opioid use raises the possibility of opioid use disorder or addiction. People who have previously experienced mental health issues or substance use disorders may be more susceptible.
- Individual health factors: The appropriateness of long-term opioid use can be influenced by age, general health, and the existence of other medical conditions.
Patients receiving long-term opioid therapy must communicate openly and continuously with their medical professionals. Frequent check-ins make it possible to evaluate how well the treatment plan is working, keep an eye out for any indications of dependence or tolerance, and address any issues or side effects.
The ultimate objective is to minimize the risks related to opioid use while achieving effective pain management. Depending on the needs and response to the treatment of the patient, medical professionals may modify treatment plans, think about tapering opioids, or investigate alternative pain management techniques.
Can You Get Addicted to Opiates in 2 Weeks?
Yes, someone can become addicted to opiates in a short period, such as two weeks. Numerous factors, such as the opioid's potency, the individual's susceptibility, and the existence of underlying risk factors, affect the likelihood of addiction. Opioids interact with the brain's reward system and can cause euphoria.
They include both illegal drugs like heroin and prescription painkillers. When opioids are taken regularly for a short while, the brain may adjust, and tolerance develops, requiring higher doses to have the same effects. Furthermore, quick exposure to opioids can result in physical dependence, where the body starts to depend on the drug to function normally.
People may experience withdrawal symptoms when they stop using opioids as their dependence worsens. Tolerance and physical dependence together increase the likelihood of addiction, which is defined by obsessive drug-seeking behavior despite drawbacks. As a result, using opioids for even a brief period can increase the risk of addiction, underscoring the significance of careful prescribing procedures, vigilant supervision, and early intervention.
Get Opioid Addiction Treatment at Banyan
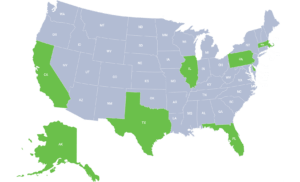
It is imperative to take proactive measures toward recovery and regaining a life free from the grip of these dangerous substances in light of the alarming rise in opioid abuse and addiction. Banyan's nationwide addiction treatment centers offer hope and healing for those who are struggling with opioid addiction, whether it be for themselves or someone they know.
Our evidence-based addiction treatment programs are made to address opioid dependence on all levels—psychological, emotional, and physical. We are dedicated to offering compassionate care that promotes long-lasting recovery and recognizes the urgency of the circumstance.